Click title or image to learn more
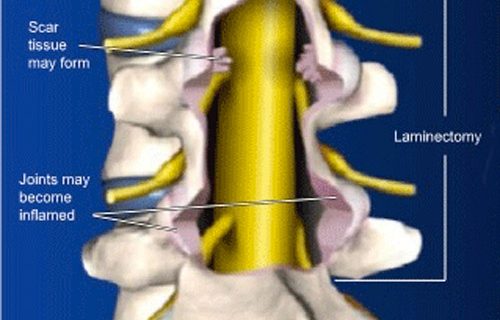
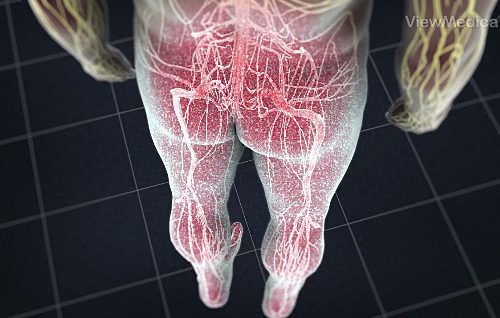
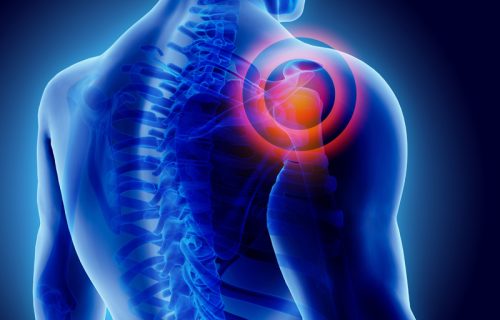
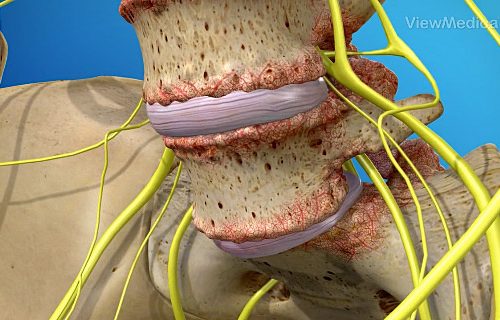
Conditions
Pain Institute of Southern Arizona and The Regional Pain Institute
Our providers understand that pain from an illness, injury or aging can disrupt a person’s activities and day-to-day routines. The team of renowned Interventional Pain Management Specialists, with training from world-class institutions such as the Mayo Clinic, Stanford and Harvard, deliver state-of-the-art treatments and procedures. Our goal is to help patients find relief from pain—helping them return to an enjoyable quality of life.
Appointments: 1-520-999-9000
General Inquiries: 1-520-318-6035
Fax: 1-520-795-9953
.


.


Tucson
1st and River
> 4582 N. 1st Avenue, Suite 140, 170, 190
> Tucson, AZ 85718
> Appointments: 1-520-999-9000
> General Inquiries: 1-520-318-6035
.
Grant and Swan
> 4881 E. Grant Road, Suite 101
> Tucson, AZ 85712
> Appointments: 1-520-999-9000
> General Inquiries: 1-520-318-6035
.
Kolb and Speedway
> 7140 E. Rosewood Street, Suite 110
> Tucson, AZ 85710
> Appointments: 1-520-999-9000
> General Inquiries: 1-520-318-6035
.
Benson
> 335 S. Ocotillo Avenue
> Benson, AZ 85602
> PH. 1-520-999-9000
The Regional Pain Institute
Queen Creek/San Tan Valley
> 36453 N. Gantzel Road, Suite 101
> San Tan Valley, AZ 85140
> PH. 1-480-636-1225
.
Apache Junction
> 750 S. Ironwood Drive, Suite 101
> Apache Junction, AZ 85120
> PH. 1-480-636-1225
©2021 Pain Institute of Southern Arizona. Website by Aztec Media